Headache Behind the Eyes is a common complaint that can range from a dull ache to severe, debilitating pain. While often alarming due to its location, it’s important to understand that this type of headache is usually a symptom pointing towards an underlying issue rather than a diagnosis in itself. The discomfort felt specifically in the retro-orbital region (the area behind your eyeballs) can stem from various sources, some directly related to the eyes, others originating from nearby structures like the sinuses, or even being manifestations of primary headache disorders.
Understanding the potential causes is the first step towards finding effective relief and managing this often disruptive symptom. This article delves into the common culprits behind a Headache Behind the Eyes, associated symptoms, when to seek medical help, and practical management strategies.
Common Causes of Headache Behind the Eyes
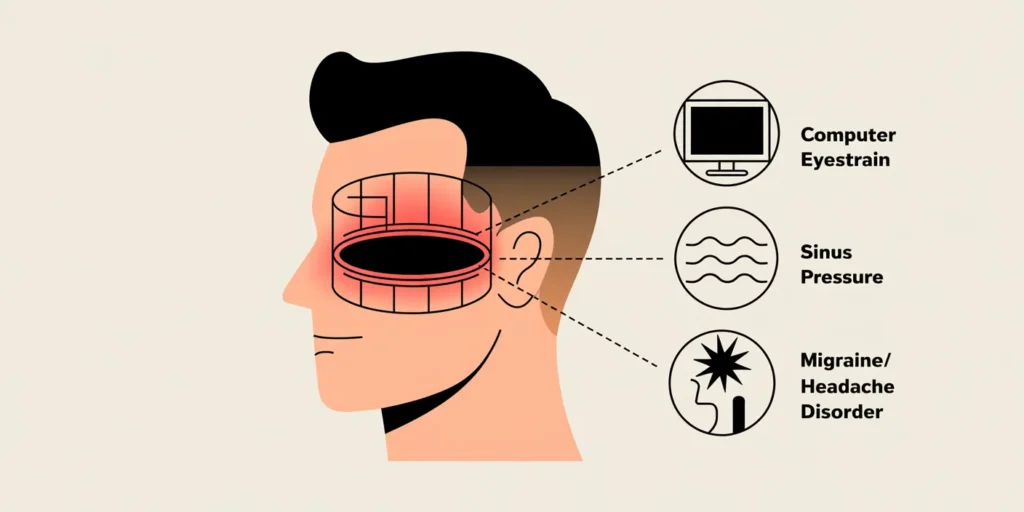
Pain perceived behind the eyes doesn’t always originate there. Several conditions can cause referred pain or direct discomfort in this sensitive area. Identifying the underlying cause is crucial for appropriate treatment.
Eye-Related Conditions
Problems directly involving the eyes or their function are frequent contributors to pain felt behind them.
- Eyestrain (Asthenopia): This is perhaps the most common cause, especially in the digital age. Prolonged focus on screens (computers, phones, tablets), reading for long periods, or driving long distances without breaks can fatigue the eye muscles. This strain often manifests as a dull ache or pressure sensation behind the eyes, sometimes accompanied by blurred vision, dry eyes, or increased sensitivity to light. Ensuring proper lighting, taking regular breaks using the 20-20-20 rule (every 20 minutes, look at something 20 feet away for 20 seconds), and using lubricating eye drops can help alleviate digital eyestrain. An outdated or incorrect glasses prescription can also lead to significant eyestrain and Headache Behind the Eyes.
- Refractive Errors: Uncorrected or poorly corrected vision problems like nearsightedness (myopia), farsightedness (hyperopia), and astigmatism force your eyes to work harder to focus, leading to muscle strain and subsequent headaches often felt behind the eyes. A comprehensive eye exam can determine if you need corrective lenses or an update to your current prescription.
- Acute Angle-Closure Glaucoma: This is a serious medical emergency. It occurs when the fluid pressure inside the eye increases rapidly because the drainage angle becomes blocked. Symptoms include severe eye pain (often described as behind the eye), blurred vision, halos around lights, nausea, and vomiting. This condition requires immediate medical attention to prevent permanent vision loss. While less common than other causes, its severity warrants awareness.
- Other Eye Issues: Conditions like Scleritis (severe inflammation of the white outer layer of the eye) or Optic Neuritis (inflammation of the optic nerve, often associated with multiple sclerosis) can also cause pain behind the eye, frequently accompanied by vision changes or pain with eye movement.
Sinus Problems (Sinusitis)
The sinuses are air-filled cavities located within the skull, including areas around and behind the eyes (sphenoid and ethmoid sinuses). When these sinuses become inflamed due to infection (viral, bacterial, or fungal) or allergies, it’s called sinusitis.
- How Sinusitis Causes Pain: Inflammation and mucus buildup increase pressure within the sinus cavities. This pressure can radiate to surrounding areas, often causing a deep, dull ache or intense pressure sensation behind the eyes, across the forehead, cheeks, or even in the upper teeth. The pain often worsens when bending forward or lying down. A Headache Behind the Eyes due to sinusitis is typically accompanied by other sinus symptoms like nasal congestion, thick nasal discharge (often yellow or green), facial tenderness, reduced sense of smell, and sometimes fever or fatigue.
- Acute vs. Chronic: Acute sinusitis develops quickly, often after a cold, while chronic sinusitis lasts for 12 weeks or more despite treatment attempts. Both can cause headaches felt behind the eyes.
Primary Headache Disorders
Sometimes, the Headache Behind the Eyes is a feature of a primary headache disorder, meaning the headache itself is the main problem, not a symptom of another condition.
- Migraine: Migraines are neurological events often characterized by moderate to severe throbbing or pulsating pain, typically on one side of the head, but the pain can certainly localize behind one or both eyes. Migraines are frequently accompanied by other symptoms like nausea, vomiting, and extreme sensitivity to light (photophobia) and sound (phonophobia). Some people experience an aura (visual disturbances like flashing lights or blind spots) before the headache phase. The pain behind the eye in a migraine can be intense.
- Tension Headaches: These are the most common type of headache globally. They usually cause mild to moderate pain described as a constant ache or pressure, often feeling like a tight band around the head. While typically felt on both sides, the pain can sometimes radiate to or be perceived primarily behind the eyes, though usually less severe than migraine or cluster headache pain. Stress, poor posture, and muscle tension are common triggers.
- Cluster Headaches: These are relatively rare but extremely severe headaches. They occur in cyclical patterns or “clusters.” The pain is excruciating, often described as a burning or stabbing sensation, typically located in or around one eye (often behind it). The affected eye may become red, watery, or droopy, and the nostril on that side might get stuffy or runny. The pain is usually unilateral and sufferers often become restless or agitated during an attack.
Understanding Your Symptoms: What Else to Look For
Pinpointing the cause of your Headache Behind the Eyes often involves paying close attention to accompanying symptoms and the characteristics of the pain itself.
Accompanying Signs
Note any other symptoms occurring alongside the headache:
- Visual Disturbances: Is your vision blurred? Do you see double? Are there new floaters or flashes of light? Is there pain when you move your eyes?
- Nausea or Vomiting: Often associated with migraines or acute angle-closure glaucoma.
- Sensitivity to Light or Sound: A hallmark of migraines.
- Facial Pressure or Tenderness: Suggestive of sinusitis. Check for pain when pressing gently on your forehead, cheeks, or the bridge of your nose.
- Nasal Symptoms: A runny or stuffy nose, or thick discharge points towards sinus involvement or potentially cluster headaches (if one-sided and watery).
- Eye Appearance: Is the eye red, watery, or is the eyelid drooping? (Common in cluster headaches or certain eye inflammations).
Pain Characteristics
Describe the pain as accurately as possible:
- Quality: Is it sharp, stabbing, dull, aching, throbbing, pulsating, or pressure-like?
- Location: Is it behind one eye or both? Does it radiate elsewhere?
- Severity: Use a pain scale (0-10) if helpful.
- Timing: When does it occur? How long does it last? Is it constant or intermittent? Does it wake you from sleep (common with cluster headaches)?
- Triggers: Does anything seem to bring it on (stress, specific foods, screen time, allergens, weather changes)?
- Relieving Factors: Does anything make it better (rest, darkness, medication, specific positions)?
Keeping a headache diary can be extremely helpful for identifying patterns and providing valuable information to your doctor.
When to Seek Medical Attention for Headache Behind the Eyes
While many headaches behind the eyes are benign, some situations warrant prompt medical evaluation to rule out serious underlying conditions.
Red Flag Symptoms
Seek immediate medical attention (visit an emergency room or call emergency services) if your Headache Behind the Eyes is accompanied by any of the following:
- Sudden, Severe Onset: A “thunderclap” headache that reaches maximum intensity within seconds or a minute, often described as the “worst headache of your life.” This could indicate a brain aneurysm or hemorrhage.
- Headache After Head Injury: Any significant headache following trauma needs evaluation.
- Fever and Stiff Neck: Could indicate meningitis or another infection.
- Neurological Symptoms: Weakness or numbness in any part of the body, difficulty speaking, confusion, personality changes, seizures, or loss of consciousness.
- Vision Loss: Sudden or significant changes in vision, especially in one eye.
- Pain That Worsens: Headaches that progressively get worse over days or weeks, or change significantly in pattern.
- New Headache Over 50: The first onset of a significant headache type after age 50 requires careful evaluation.
- Pain with Chewing: Jaw claudication can be a sign of temporal arteritis.
- Systemic Symptoms: Unexplained weight loss, night sweats, or general malaise alongside the headache.
Diagnosis Process
If your headache is persistent, severe, or concerning, consult your doctor. They will likely:
- Take a Detailed Medical History: Asking about your symptoms, headache patterns, triggers, family history, and overall health.
- Perform a Physical and Neurological Exam: Checking vital signs, coordination, reflexes, sensation, and mental status.
- Conduct an Eye Examination: Checking vision, eye pressure, eye movements, and looking at the structures inside your eye (fundoscopy). This is crucial for identifying eye-related causes.
- Order Imaging Tests (If Necessary): CT scans or MRIs of the brain and sinuses may be ordered if a serious underlying cause (like a tumor, aneurysm, or complex sinusitis) is suspected based on your history or exam findings.
Managing and Treating Headache Behind the Eyes
Treatment focuses on addressing the underlying cause, managing symptoms, and preventing future occurrences.
Home Remedies and Lifestyle Adjustments
For milder headaches, especially those related to eyestrain or tension:
- Rest and Hydration: Sometimes simply resting your eyes in a dark, quiet room and ensuring adequate fluid intake can help.
- Over-the-Counter (OTC) Pain Relievers: Medications like ibuprofen, naproxen, or acetaminophen can provide temporary relief for mild to moderate pain. However, avoid overuse, as this can lead to medication-overuse headaches.
- Cold or Warm Compresses: Applying a cold pack or cool cloth over the eyes and forehead can help numb the area and constrict blood vessels (often helpful for migraines). A warm compress over the face might soothe sinus pressure. Experiment to see what works for you.
- Manage Screen Time: Implement the 20-20-20 rule consistently. Adjust screen brightness and contrast. Consider blue light filtering glasses. Ensure your workstation ergonomics are correct (screen at eye level, proper distance).
- Stress Management: Practice relaxation techniques like deep breathing, meditation, yoga, or gentle exercise. Identify and manage stressors in your life.
- Adequate Sleep: Aim for a consistent sleep schedule and 7-9 hours of quality sleep per night.
- Check Your Environment: Ensure good lighting for reading and working. Avoid known triggers like strong smells or allergens if applicable.
Medical Treatments (Based on Cause)
Treatment tailored to the specific diagnosis is key:
- Eyestrain/Refractive Errors: An updated glasses or contact lens prescription is often the solution. Artificial tears can help with dryness.
- Sinusitis: Treatments may include nasal decongestants, saline nasal rinses, corticosteroid nasal sprays to reduce inflammation, antibiotics (if bacterial infection is confirmed), or allergy medications. In persistent cases, procedures to drain the sinuses might be considered.
- Migraine: Treatment involves abortive medications (taken at the onset of a migraine to stop it, like triptans or CGRP inhibitors) and preventive medications (taken regularly to reduce frequency and severity). Identifying and avoiding triggers is also crucial.
- Tension Headaches: OTC pain relievers, stress management, physical therapy, and sometimes prescription medications like amitriptyline can help.
- Cluster Headaches: Treatment often involves high-flow oxygen inhalation and specific medications like triptans (often via injection or nasal spray for rapid relief). Preventive medications are also used.
- Glaucoma/Other Eye Conditions: Require specific treatments prescribed by an ophthalmologist, which may include eye drops to lower pressure or medications/procedures to manage inflammation.
Experiencing a Headache Behind the Eyes can be unsettling, but it’s often manageable once the underlying cause is identified. From simple eyestrain easily corrected with breaks and proper eyewear, to sinus pressure needing decongestion, or primary headaches like migraines requiring specific treatment plans, the range of possibilities is broad. Pay close attention to your body – note the exact nature of the pain, any accompanying symptoms, and potential triggers. While home remedies and lifestyle adjustments can provide relief for many, never hesitate to seek professional medical advice, especially if the pain is severe, sudden, persistent, or accompanied by any red flag symptoms. Diagnosing the root cause is paramount for effective and safe management. Remember, you don’t have to simply endure the pain; understanding it is the first step toward finding lasting relief.
Have you experienced a persistent Headache Behind the Eyes? What strategies or treatments have worked best for you? Share your experiences and tips in the comments below – your insights might help others navigate this common issue!

